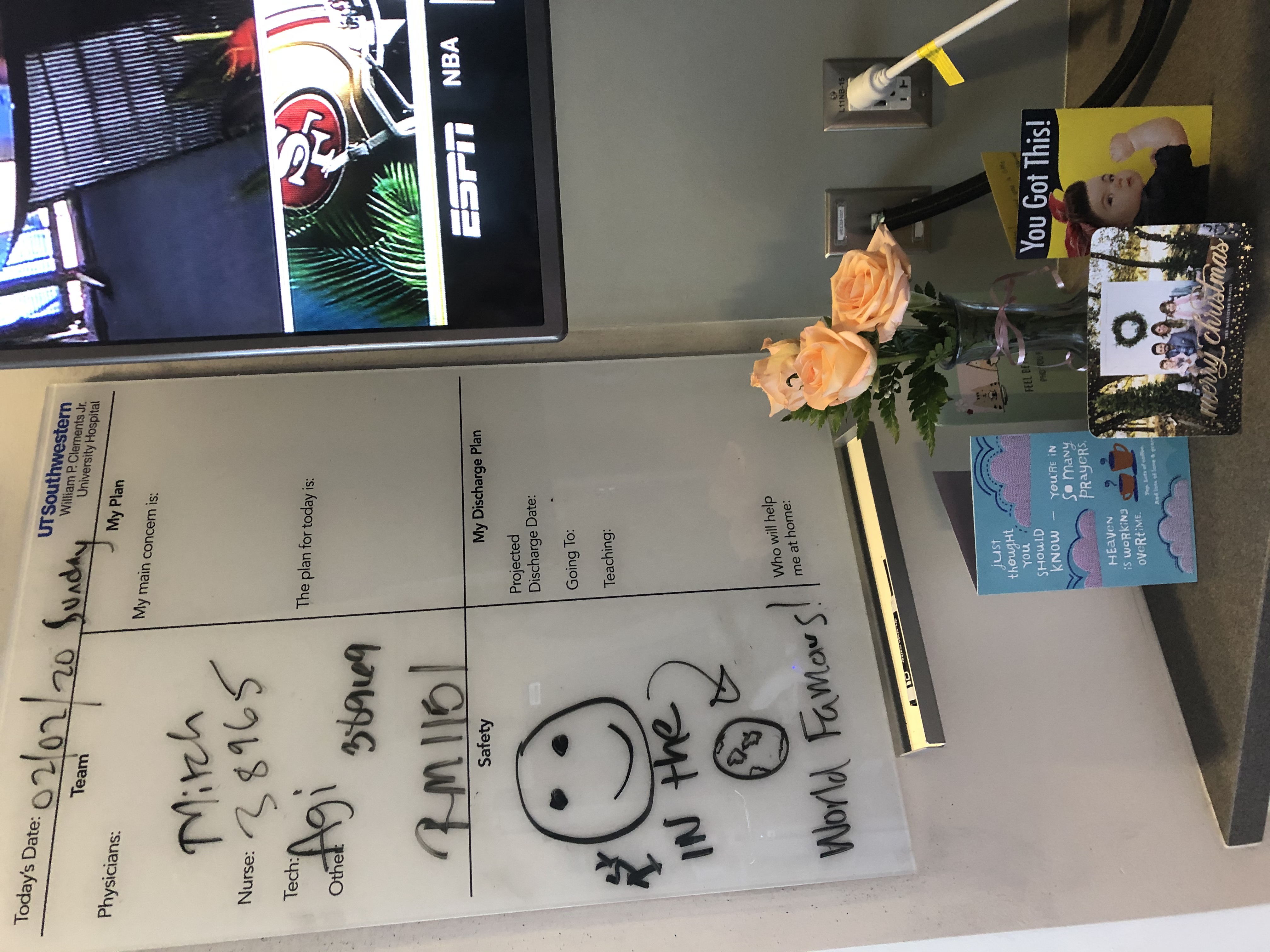
My surgery was scheduled for 7:00 am; we had to arrive at the hospital 2 hours early for check-in. My husband, Michael, and my mom were there to help get me admitted and offer moral support. My dad was at home watching our two daughters. The hospital staff was minimal. Typically, surgeries are not scheduled on a Saturday; they had purposely scheduled mine for a Saturday to minimize the number of people around, being that this would be the first robotic procedure.
The nurse who checked me in was named Carol and she was exactly what I needed that morning — bubbly, light, happy and made me feel comfortable. I anxiously watched the clock. I got my IV and made a joke about how scared I am of IVs, but alas, the lady screws up my IV and it doesn't go correctly in my hand, so she has to do it a second time in my forearm… see, I do have a reason to be scared of those!
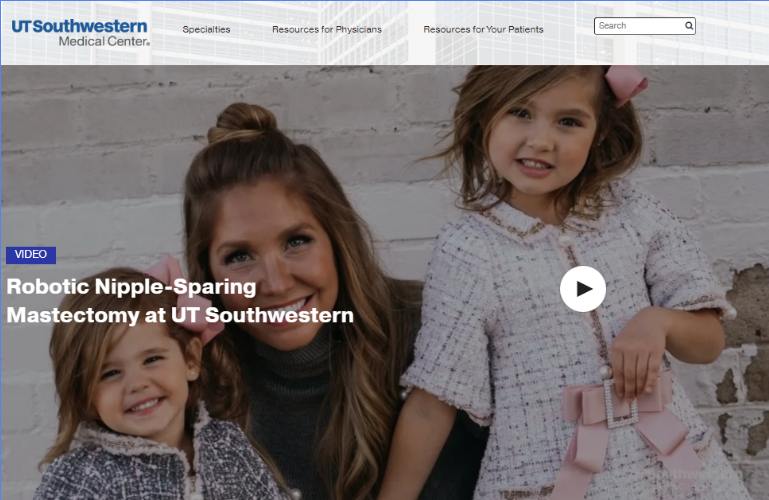
Dr. Farr finally came in to greet me. I'll never forget she had goggle marks on her face. I'll find out later that she got minimal sleep and was already up practicing for hours, hence the goggle marks. She reviews the procedure again and gives me more paperwork to sign specifically regarding the clinical trial. But then she uttered something I had not heard yet: "You will actually be the first patient in the world to have this procedure"… excuse me, come again?!
So, the 'world' comment obviously threw me, scared me, and it made me cry a little. I was aware I was their first patient, but not the first one in the world. A few chin quivers later: "excuse me, I'm just a little nervous"… OK, not computing right now, let's just do this.
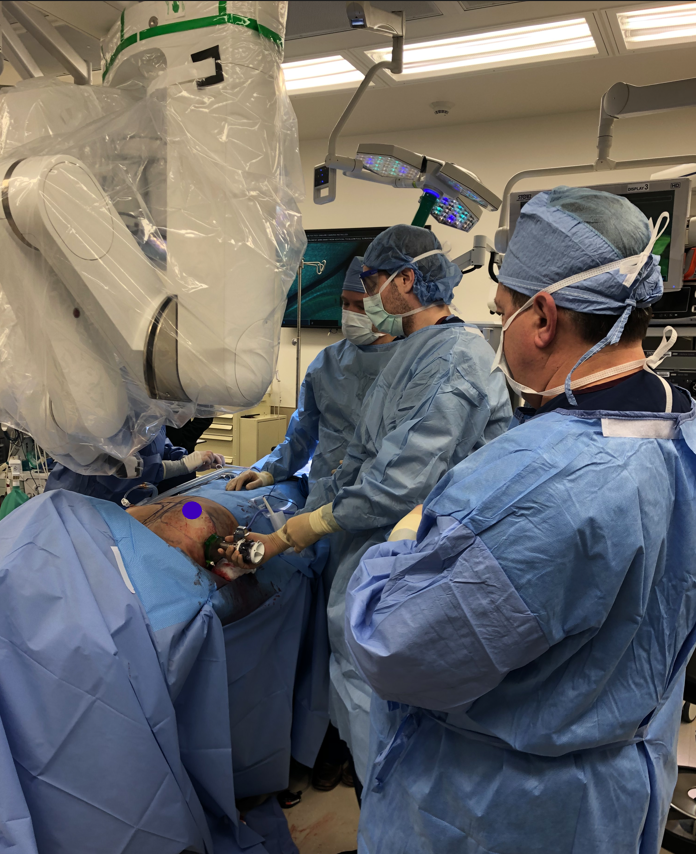
Dr. Haddock, my plastic surgeon, then had his turn. He also had me sign a consent form. Then it was time to mark me up! He had me stand up and drew with dark markers around my breasts to create a map for both him and Dr. Farr. After this, the anesthesiologist team came in and gave me anti-anxiety medicine — it was needed! I looked up and it was just about 7:00 am on the dot when they rolled me back.
I only briefly remember the actual operating room. The nurse told me she would take good care of me and they told me I had pretty eyelashes (aww, thanks!) and that was it! I would be asleep for the next 6 hours.